Object: The value of extent of resection (EOR) in improving survival in patients with glioblastoma multiforme (GBM) remains controversial. Specifically, it is unclear what proportion of contrast-enhancing tumor must be resected for a survival advantage and how much survival improves beyond this threshold. The authors attempt to define these values for the patient with newly diagnosed GBM in the modern neurosurgical era.
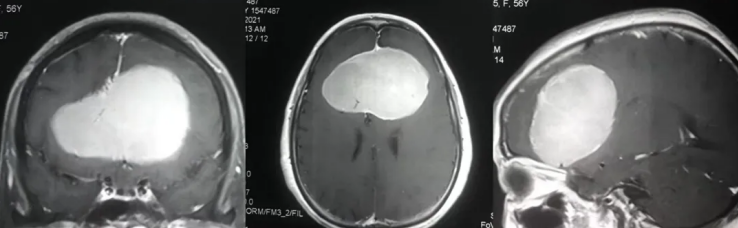
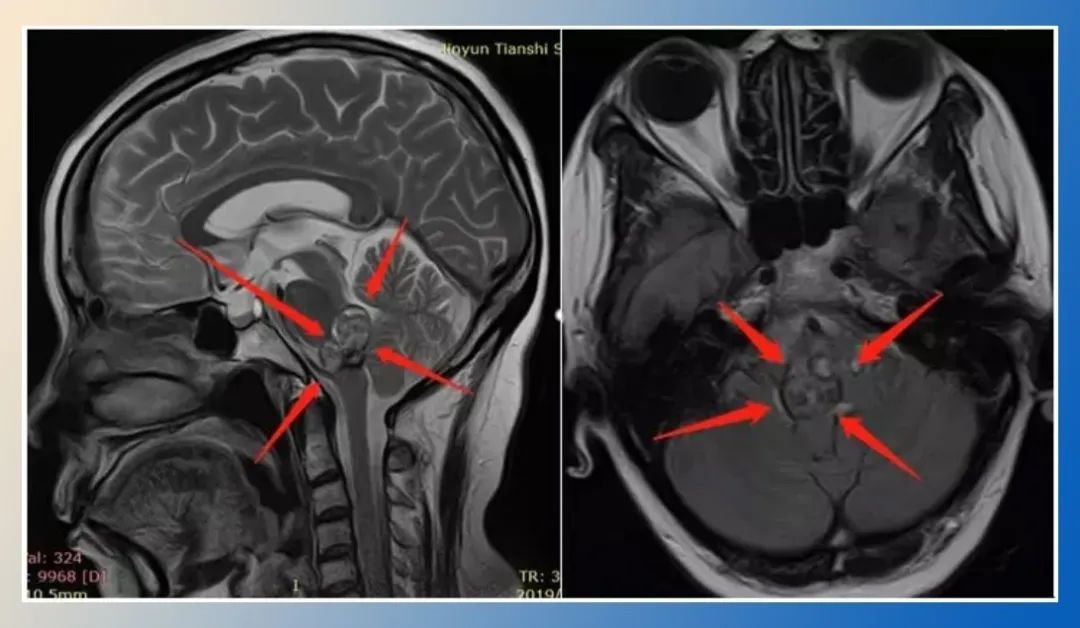
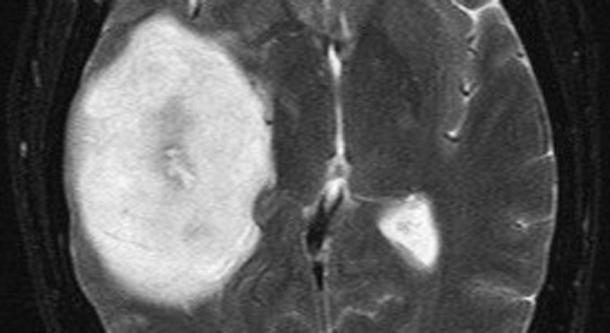
Methods: The authors identified 500 consecutive newly diagnosed patients with supratentorial GBM treated at the University of California, San Francisco between 1997 and 2009. Clinical, radiographic, and outcome parameters were measured for each case, including MR imaging-based volumetric tumor analysis.
Results: The patients had a median age of 60 years and presented with a median Karnofsky Performance Scale (KPS) score of 80. The mean clinical follow-up period was 15.3 months, and no patient was unaccounted for. All patients underwent resection followed by chemotherapy and radiation therapy. The median postoperative tumor volume was 2.3 cm(3), equating to a 96% EOR. The median overall survival was 12.2 months. Using Cox proportional hazards analysis, age, KPS score, and EOR were predictive of survival (p < 0.0001). A significant survival advantage was seen with as little as 78% EOR, and stepwise improvement in survival was evident even in the 95%-全切 EOR range. A recursive partitioning analysis validated these findings and provided additional risk stratification parameters related to age, EOR, and tumor burden.
Conclusions: For patients with newly diagnosed GBMs, aggressive EOR equates to improvement in overall survival, even at the highest levels of resection. Interestingly, subtotal resections as low as 78% also correspond to a survival benefit.
目标:多发性胶质母细胞瘤(GBM)患者切除范围(EOR)在提高生存率方面的价值仍存在争议。具体而言,目前尚不清楚需切除多大比例的造影剂增强的肿瘤才能获得生存优势,以及超过这个阈值后生存率能提高多少。作者试图为现代神经外科时代新诊断的GBM患者定义这些数值。
方法:作者确定了1997年至2009年期间在加州大学旧金山分校治疗的500例连续新诊断的脊柱上GBM患者。对每例患者的临床、放射学和结果参数进行测量,包括基于MR成像的肿瘤体积分析。
结果:患者的中位年龄为12岁。患者的中位年龄为60岁,Karnofsky表现量表(KPS)中位数为80分。平均临床随访时间为15.3个月,没有患者下落不明。全部患者均进行了切除术,然后进行化疗和放疗。术后肿瘤体积中位数为2.3 cm(3),相当于96%的EOR。中位总生存期为12.2个月。使用Cox比例危险分析,年龄、KPS评分和EOR对生存有评估作用(P <0.0001)。在EOR为78%时就能看到的生存优势,即使在95%-全切的EOR范围内,生存率的阶梯式好转也很明显。递归分区分析验证了这些发现,并提供了与年龄、EOR和肿瘤负担相关的额外风险分层参数。
结论:对于新诊断的GBMs患者,的EOR相当于好转总生存期,即使在较高水平的切除。有趣的是,低至78%的次总切除也对应着生存获益。
原文链接:https://www.sci-hub.se/10.3171/2011.2.jns10998
- 文章标题:INC美国Mitchel Berger教授:新诊断胶质母细胞瘤的切除阈值范围
- 更新时间:2020-11-05 10:55:57

 400-029-0925
400-029-0925